Narcissistic personality disorder DSM-5
- Category Diagnosis of Narcissistic personality disorder DSM-5
Narcissistic personality disorder
(DSM-5)
A persistent pattern of grandiosity (in conduct or fantasy), a constant desire for admiration, and a lack of empathy are features of narcissistic personality disorder DSM.5 (NPD), a cluster B personality disorder.
Signs and symptoms of Narcissistic personality disorder DSM-5
The American Psychiatric Association defines NPD in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) as a pervasive pattern of grandiosity (in fantasy or behavior), a constant need for admiration, and a lack of empathy that begins in early adulthood and manifests in a variety of contexts:
- A great sense of self-importance
- Obsession with illusions of unending success, dominance, genius, beauty, or ideal love
- A conviction that one is unique and special and that one should associate with or be understood by other elite or highly-regarded individuals or groups
- A desire for overwhelming adoration
- Possession of a sense of entitlement
- Interpersonal exploitation of others
- A lack of compassion.
- The feeling that someone else is envious of him or her.
- A sign of arrogant and boastful attitudes or actions.
According to a proposed alternative model described in the DSM-5, NPD is defined as moderate or more impairment in personality functioning, demonstrated by issues in two or more of the following four areas:
- Identity
- Self-direction
- Empathy
- Intimacy
Grandiosity and attention-seeking are also present in NPD, which makes it distinct from other mental disorders.
Although there are no clear-cut physical signs that may be used to detect NPD, there may be physical signs of substance addiction, which is usually linked to NPD. A mental status examination may reveal a depressed state. Patients with narcissistic grandiosity may have maniacal or hypomanic symptoms.
Diagnosis of Narcissistic personality disorder DSM-5
The other three cluster B personality disorders, which are as follows, must be distinguished from NPD:
- Antisocial Personality Disorder (ASPD)
- Borderline Personality Disorder (BPD)
- Histrionic Personality Disorder (HPD)
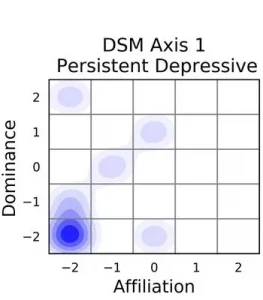
NPD individuals may also meet the criteria for other axis diseases. Alternatively, people with only NPD may occasionally show symptoms similar to those of axis I illnesses.
There are no specific laboratory tests used to diagnose NPD, while a toxicology screen is recommended to rule out alcohol and drug use as probable pathology-causing factors.
Despite substantial debate about their validity and reliability, the following personality tests may be used to assess character disorder and aid in the diagnosis of NPD:
- Personality Diagnostic Questionnaire–4 (PDQ-4)
- Millon Clinical Multiaxial Inventory III (MCMI-III)
- International Personality Disorder Examination (IPDE)
Management
The preferred treatment strategy is long-term, regular outpatient care, which typically includes a mix of psychotherapy and medication administration.
Psychotherapy options include the following:
Individual psychotherapy (especially psychoanalytic psychotherapy) – The cornerstone of treatment; schools of thought include Kernberg’s object-relations method and Kohut’s self-psychology approach, as well as countless combinations of the two.
- Group therapy
- Family therapy
- Couples therapy
- psychological counseling (CBT; in particular, schema-focused therapy)
- Short-term objective-focused psychotherapy
If the patient acutely decompensates or poses a risk to themselves or others, inpatient therapy (for a limited time) may be required.
There are no psychiatric medications specifically intended to treat NPD. Patients with this illness frequently benefit from the use of psychiatric medicines to treat concomitant axis I diagnoses or to deal with some of the symptoms associated with the disorder. Agents such as the ones listed below could be suggested:
- selective serotonin reuptake inhibitor (SSRI) class antidepressants (eg, citalopram)
- Antipsychotics (eg, risperidone)
- Mood stabilizers (eg, lamotrigine)
Narcissistic Personality Disorder Treatment & Management
Approach Considerations
Long-term, continuous outpatient care is the best treatment option for narcissistic personality disorder (NPD). This is usually accomplished through a combination of psychotherapy and medication delivery.
The cornerstone of treatment is individual psychotherapy, primarily psychoanalytic psychotherapy. Other therapeutic strategies used to treat the condition, in addition to CBT and short-term objective-focused psychotherapy, including group, family, and couples therapy. Although psychotropic medicines are routinely used to address concurrent anxiety, depression, impulsivity, or other mood disorders, they are not specifically prescribed to treat NPD.
Inpatient care is required if the patient decompensates rapidly or poses a risk to himself or others. Patients with NPD often benefit from shorter hospital stays because longer stays do not change the severity of the disease at its core. When hospitalization is required, only temporary remedies such as lowering medication dosages or stabilizing environmental stressors should be used.
Psychotherapy
Although individual psychoanalytic psychotherapy is the primary strategy for treating NPD, experts vary on the optimum course of action. The two basic schools of thought in this field are Otto Kernberg’s object-relations approach and Heinz Kohut’s self-psychology approach, and each offers a unique and at first appears incongruous strategy for treating narcissistic patients.
A therapist’s role, according to Kernberg’s theory, is to actively interpret the patient’s narcissistic defenses while also shedding light on the patient’s negative transferences. Kernberg believed that by confronting the patient directly, the diseased grandiose ego could be eliminated or diminished.
Kohut, on the other hand, advocated a more sympathetic method in which the therapist actively supported the patient’s arrogance and aided the development of idealization in the transference. Kohut’s ultimate goal was to strengthen the patient’s self-structure, which was fundamentally weak.
There have been no conclusive studies recommending one therapy strategy over another. Currently, the majority of physicians prefer a hybrid of the two. Most people prefer a flexible, moderate approach that carefully evaluates the patient’s narcissistic defenses while also empathically acknowledging their need for them.
By this method, the therapist should recognize the self-preservation function that narcissism performs in the patient’s daily life and exercise caution when removing narcissistic obstacles.
At the same time, the therapist should attempt to assist the patient to develop a realistic understanding of his or her behavioral flaws.
In addition to individual psychodynamic psychoanalysis, NPD has been treated with group therapy and CBT. Initially, therapists assumed that narcissistic patients couldn’t handle the essential give-and-take of group therapy, making it improper for them.
This initial assumption that group therapy was wrong was correct since group processes often need empathy, tolerance, and the ability to relate to and connect with others—qualities that narcissists lack.
Long-term group therapy, on the other hand, has been demonstrated in studies to aid narcissistic patients by providing a safe atmosphere in which they can experiment with boundaries, take criticism, create trust, and become more self-aware.
CBT may also be beneficial for narcissistic patients. The purpose of schema-focused treatment, a kind of CBT, is to repair narcissistic schemas as well as the dysfunctional moods and coping processes that they are associated with. Because CBT forces patients to address narcissistic cognitive distortions, it has yielded some promising results in the treatment of NPD (such as perfectionism and black-and-white thinking).
Pharmacologic Therapy
There are no psychiatric medications specifically intended to treat NPD. However, people with this problem frequently benefit from taking psychiatric medicines to help manage some of the disorder’s symptoms (eg, depression, anxiety, transient psychosis, mood lability, and poor impulse control). Many NPD patients also have axis I problems for which they receive psychiatric treatment regularly. The following drugs may be used to treat NPD patients:
- Antidepressants of the selective serotonin reuptake inhibitor (SSRI) class (eg, citalopram)
- Antipsychotics (eg, risperidone)
- Mood stabilizers (eg, lamotrigine)
Long-Term Monitoring
Patients with NPD can suddenly become suicidal, even when they are not visibly depressed, making it difficult for clinicians to predict the risk of suicide in these patients. Acute narcissistic insults, which cut to the core of a person’s poor self-esteem, can cause narcissistic patients to respond recklessly and dangerously.
Therefore, it is critical that the doctor continuously watch the NPD patient, keeping a constant eye out for any unforeseen life events that can catch the patient off guard. In addition, the patient’s access to drugs and firearms that could be used as suicide weapons should be restricted. To assist the patient and safeguard the therapist from any potential legal action, the clinician should meticulously document every aspect of the patient’s course of therapy, just like in any therapeutic interaction.
Medication Summary
Although no psychiatric pharmaceuticals are specifically approved for the treatment of narcissistic personality disorder (NPD), patients frequently benefit from utilizing such medications to help control concomitant axis I disorders or to alleviate some of the symptoms associated with this disorder. Some medicines that may be considered are antidepressants (particularly, selective serotonin reuptake inhibitors [SSRIs]), antipsychotics, and mood stabilizers.
Comparison to other personality disorders
NPD and borderline personality disorder share characteristics such as societal stigma, unclear origins, and prevalence rates. According to a study published in 2020, NPD is following in the footsteps of borderline personality disorder: “Over the last three decades, great progress has been made in understanding the psychopathology, longitudinal course, and viable therapies for BPD. NPD, which is still stigmatized and understudied in the same manner that BPD was previously, holds the potential for a new wave of research and treatment advances.”
NPD is akin to the now-debunked “multiple personality disorder” (MPD) personality constellation in popular culture and clinical mythology. MPD had major mainstream media attention in the 1980s, but it was all but forgotten in public debate during the next two decades because many of its claims had been comprehensively debunked and its introduction into the field of legal defense had caused harm to society.